Cervicocephalic syndrome
Introduction
Cervicocephalic syndrome (CCS) includes pain and stiffness of the upper cervical spine with associated headache. The syndrome frequently demonstrates symptoms of dizziness and often visual (e.g. nystagmus) or auditory disturbances (e.g. tinnitus).
This term is outdated and not commonly used in clinical practice, although it may still be used in some parts of the world.
Definition / Description
These symptoms may be related to vertebrobasilar insuffisiency where interference with the blood flow in the vertbral artery occurs when the neck is inclined to one side, rotated or extended.
Clinically Relevant Anatomy
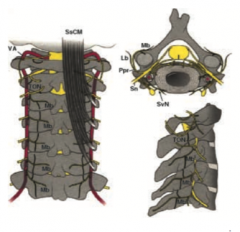
The upper cervical complex consists of the atlanto - ocipital(jointC0-C1), the atlanto-axial (1joint-C2) and the superior aspect of C2.
The vertebral arteries begin in the root of the neck. Usually the left artery is larger than the right. The cervical parts of the vertebral arteries ascend through the transverse foramina of the first six cervical vertevrae. The dura and arachnoid is perforated by the atlantic parts of the vertebral arteries that pass through the foramen magnum. At the caudal border of the pons, the basilar artery is formed out of the intracranial arteries of the vertebral arteries
Epidemiology /Etiology
Cervicocephalic syndrome is often a mixed syndrome caused by spondylogenic irritation and actual compression.
The essential factors are:
- irritation of sensory nerve fibers, rarely of motor and autonomic fibers
- irritation or compression of the vertebral artery
- irritation of greater and lesser occipital nerves
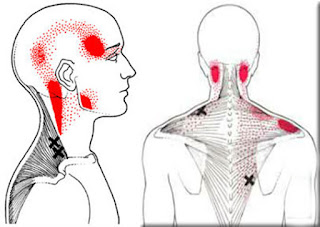
Impingement on the vertebral artery and the sympathetic nerve near the cervical spine can be related to cervicocephalic syndrome. By stimulation of nociceptors in zygapophyseal joints, symptoms in nearby muscles and tendons can be stimulated. This impingement could be caused by malpositioned joints at the head/neck junction, deviations of the cervical spine from the body axis, displacement of vertebrae and constriction of the vertebral artery
Characteristics/Clinical Presentation
Cervical headaches affect approximately 2.5% of the adult population and comprise roughly 15 to 20% of all chronic and recurrent headaches. Headache and neck pain are the two most common complaints reported by patients with cervicocephalic syndrome. Other symptoms associated with the syndrome include dizziness, auditory disturbance and visual disturbance.
Cervicocephalic kinesthetic sensibility is a common complaint related to chronic neck disorders, mostly accompanied with a decreased postural balance. The ability to accurately recognise movements in the neck is reduced due to disturbed proprioception.
Differential Diagnosis
Many diseases cause headache therefore thorough evaluation and differential diagnosis is important. General causes of headache (e.g. metabolic disease, hypertension and visual disturbance) can be ruled out quite easily. CCS is sometimes incorrectly diagnosed as migraine but the two conditions differ in many ways. Common migraine differs from cervicocephalic migraine in duration of each attack as well as the corresponding symptoms such as vomiting and nausea. Other symptoms (dizziness and vestibular disturbances) related to cervicocephalic syndrome can be provoked or worsened by movements of the head and cervical spine, unlike symptoms associated with non-cervicogenic dizziness and vestibular disturbances.
Pathologies that may present similarly to cervicocephalic syndrome include;
- Disc herniation
- Spondylotic bony compression
- Spinal cord syndrome
- Tumor metastases
Diagnostic Procedures
The Cervicogenic Headache Study Group established the following criteria for the diagnosis of CH: Provocation by head movements, maintenance of antalgic head posture and (partial) relief of pain by diagnostic blockade. Because CCS comprises of cervicogenic headache, the preconceived criteria are therefore of use in the diagnostic procedure of CCS. Complaints such as dizziness and vestibular disturbances arouse with certain head movement as said in previous subtitles.
Outcome Measures
Patients who followed a proprioceptive rehabilitation programme improved a significant in controlling head repositioning accuracy compared with a control group who did not follow this program. However, it is not clear if the difference in reposition angle also has clinical relevance (2 degrees). Clinical parameters such as pain, analgesic intake, ROM and daily functioning are also improved significantly in the intervention group.
Examination
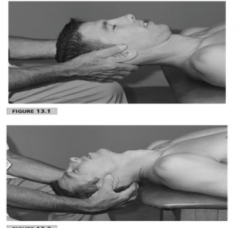
Rule out vertebral artery dissection
The sensibility of head orientation can be evaluated by relocating the head after an active movement. When performing this test, the patient is asked to relocate his/her head after an active rotation to the left and right. When healthy persons and patients are compared, the patient group demonstrates significantly worse scores on this test. The validity and test-retest reliability demonstrate an excellent result for measuring the cervical proprioception.
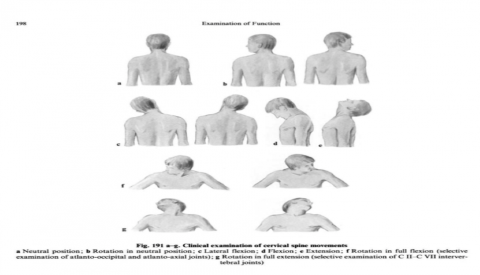
Cervicocephalic kinesthesia tests were also used to measure cervical ROM, since moderate- substantial test-retest reliability has been reported for measurements of cervical mobility.
There are five tests to determine the cervicocephalic kinaesthesia. It is clear that patients with cervicocephalic syndrome have more difficulties to relocate the head to a neutral head posture and to repeat head movements (figure eight movement). The test may be divided into two categories:
- NHP
- uncommon postures and movements.
These tests are reliable and have a good IC.
Tests of cervicocephalic kinaesthesia
The movement of axial rotation was chosen as the predominant test movement as humans use rotation most commonly in exploring the external environment.
Test 1: Relocation to the NHP (natural head posture). The starting position was sitting with the head in NHP. Subjects were asked to perform full active cervical rotation to the left and right in turn and then to return and indicate when they considered they had relocated the starting position as accurately as possible.This point was recorded by activation of the electronic marker switch. Between each test movement, the subject’s head was manually adjusted back to the original starting position by the principal researcher who was guided by the real-time computer display. The examiner’s accuracy in relocating subjects’ heads was within ±0.2˚, as indicated by the marker,which changed colour from red to green when the accuracy was within the set limits.
When healthy persons and patients are compared, the patient group indicates significantly worse scores on the test[2]. The validity and test-retest reliability demonstrate an excellent result for measuring the cervical proprioception[4].
When healthy persons and patients are compared, the patient group indicates significantly worse scores on the test[2]. The validity and test-retest reliability demonstrate an excellent result for measuring the cervical proprioception[4].
Test 2: Relocation to the 30˚ rotation position and to NHP. In this test, the examiner pre-positioned the subject’s head in 30˚ left rotation and subsequently in right rotation. The computer visual display unit guided the researcher. A marker was placed to indicate the 30˚ position. Subjects were permitted to concentrate on this position of reference for a few seconds. They then turned their head to NHP and then returned to the 30˚ rotation position. Recordings were taken on each occasion subjects returned to the NHP and to the 30˚ position.
Test 3: Preset trunk rotation Subjects sat on a chair positioned on a specially constructed platform. A familiarization session was conducted before the formal test. Subjects first concentrated on their NHP. Whilst the researcher held the subject’s head steady, the platform (and therefore the subject’s trunk) was rotated to a pre-marked 30˚position of left rotation. Subjects were required to relocate their NHP with respect to the body and then return to the starting position (30˚ relative neck rotation). Following three trials in left trunk rotation, the test was repeated with the trunk rotated to the right.
Test 4: Figure-of-eight relocation test. Subjects were taught to perform a discreet figure-of-eight movement by moving the head. As a guide, a 10-cm diameter diagram of a figure-of-eight lying on its side was placed on a stand one metre in front of the subject. Subjects were instructed to trace the figure-of-eight with their nose toconfine movement predominantly to the upper cervical spine. Each subject was permitted three practice trials of the movement with their eyes open. The examiner corrected the performance if the movement was too little or too large, that is, involving the lower cervical spine. In the formal test,subjects performed the movement three times and, after each trial, were required to relocate to the start position as accurately as possible.
Test 5: Figure-of-eight movement test. In this test, subjects repeated the figure-of-eight movement three times, without stopping, as consistently as possible. Each time a crossover was made in the figure-of-eight movement, subjects were asked to pass through their NHP as accurately as possible. They therefore crossed the starting position five times in the test sequence.There was no practice in advance of this test.
Medical Management
Medication
Because this condition occurs on a biomechanical level, the role of medication is purely symptomatic. No evidence is found for influence of the drugs on the volume or consistency of the cervical discs. Despite this fact medication has been proven to be effective because it relieves the patient of his deep and severe pain. Also sedatives and tranquillizers can be used. Those can lessen the central sensitization of the biomechanical stress. They can also help relieving the night pain which prevents the patient from having not only physical but also emotional stress. The therapy benefits from these results. Important is that medication is only used as an asset to the physical therapy.
They can also help relieving the night pain which prevents the patient from having not only physical but also emotional stress. Night pain and emotional stress are in relation to each other because the patient might feel stressed before going to sleep that he/she will have night pain and have a restless and painful night again. Night pain means also that the patient doesn’t sleep enough during night which is another reason to sense emotionally stressed. the therapy benefits from these results.
It is important that the patient is well-informed and has a say in the therapy because misuse of these drugs is very dangerous.
The use of local anaesthetics or steroids can be indicated when the above-mentioned medication and heat do not relieve pain and/or muscle spasm.
- Local Muscle infiltration
- Cervical epidural injection
- Cervical sympathetic and radicular blockade
Surgery
In exceptional cases when conservative therapy does not work, surgery can be applied to help patients with chronic and recurrent cervicocephalic syndrome and unbearable pain.
Percutaneous drill resection is an effective technique with a reported 85–95% success rate. Using a radiofrequency (FR) generator, an alternative heats the tissue and destroys it. The target temperature is between 60-100 degrees.
CT-guided radiofrequency thermocoagulation is an effective, precise, secure, minimally-invasive treatment for non-radicular cervical pain caused by zygapophysial joint arthropathy, when CT-guided, lateral drug instillation does not cause a lasting improvement.
Our to use radiofrequency to limit recurrences and complications that we had observed with PDR, such as skin necrosis.
Physical Therapy Management
- Manipulation: There is moderate evidence for manipulation when this technique is combined with mobilisation of the cervical spine. When manipulation is compared with an active control treatment, there is only low evidence for pain relief and improvement in function. Thoracic manipulation could be an additional therapy for pain relief.
- Mobilisation: There is little evidence for improvement when only mobilisations are performed during the therapy. There is no difference compared with acupuncture for acute pain reduction
- Exercise: Stretching and strengthening of the cervical region and the areas around it shows a moderate quality of evidence in pain reduction and improvement in function on short term to intermediate follow-up. There is low quality evidence (one trial with two publications, 24 participants) that general fitness training exercises may have no difference in pain when compared with a reference intervention (not offered any physical therapy but received health counseling on a group level and an individual level with regard to workplace ergonomics, diet, health, relaxation and stress management for a total of up to 1 hour per week) for (sub)acute/chronic neck pain immediately post-treatment.
- Electrotherapy: Very low to low evidence is available that TENS, EMS, pulsed electromagnetic field therapy and repetitive magnetic stimulation show a greater therapy effect compared with a placebo treatment
- Patient education: Education regarding the positive effects of physical exercise is important to improve adherence and satisfaction.
- Traction: A review based on 7 RCT’s shows no significant difference in pain reducation and daily functioning when a traction therapy (Mechanical traction 'stretches' the neck. With the patient lying on their back, a head halter is placed under the back of the head and possibly the jaw and attached to a machine. The machine is set for a certain time period and specific weight for the pulling action to occur. The traction can remain on steadily for the specified time (referred to as continuous or static) or intermittently (on/off cycle) during the treatment) is compared with a placebo traction.
- Endurance training:
Moderate quality evidence (one trial, 198 participants) shows moderate benefit for pain relief immediately post intervention using scapulothoracic/UE endurance training for (sub)acute/chronic mechanical neck disorders. A clinician may need to treat four people to achieve this type of pain relief. More research is needed.
- Stretching:
There is low quality evidence (one trial, 16 participants) that stretching exercises, either before or after a manipulation, made no difference on pain and function when compared with that same manipulation for chronic neck pain immediately post treatment.
- Neuromuscular exercises:
We are uncertain whether eye-neck co-ordination exercises improve pain or function. Very low quality evidence (one trial, 60 participants) shows a moderate reduction in pain and improved function in chronic neck pain in the short term for eye-neck coordination exercises. A clinician may need to treat four people to achieve this type of pain relief and three to achieve this functional benefit in one person.
For example:
- Reposition of the head while the eyes are closed
- Reposition of the head while the physiotherapist provides some resistance
- Reposition of the shoulders while holding the head is held in neutral
- Reposition of the shoulders while the eyes are closed
Clinical Bottom Line
Cervicocephalic syndrome is associated with deep or superficial pain in the head, dizziness and often auditory or visual disturbances (e.g. nystagmus, tinnitus) caused by spondylogenic irritation and actual compression resulting in pain and restriction of motion of the upper cervical spine. The head relocation test is one of the best tests to examine if a person has cervicocephalic syndrome. In terms of physiotherapy, there is low evidence for pain relief with manipulation, mobilisation, exercise therapy (stretching, strengthening, general fitness), electrotherapy, education and neuromuscular exercises. More research is needed in this area to focus specifically on cervicocephalic syndromes and the most effective therapy treatments for this condition.




Comments
Post a Comment